Polyvagal Theory Simplified: Understanding Your Nervous System
Polyvagal theory explains why you freeze when you should run, why deep breaths actually calm you, and why feeling safe is a physical experience—not just a mental one.
Developed by Stephen Porges, this theory has transformed how we understand stress, trauma, and regulation. Here's what you need to know, explained simply.
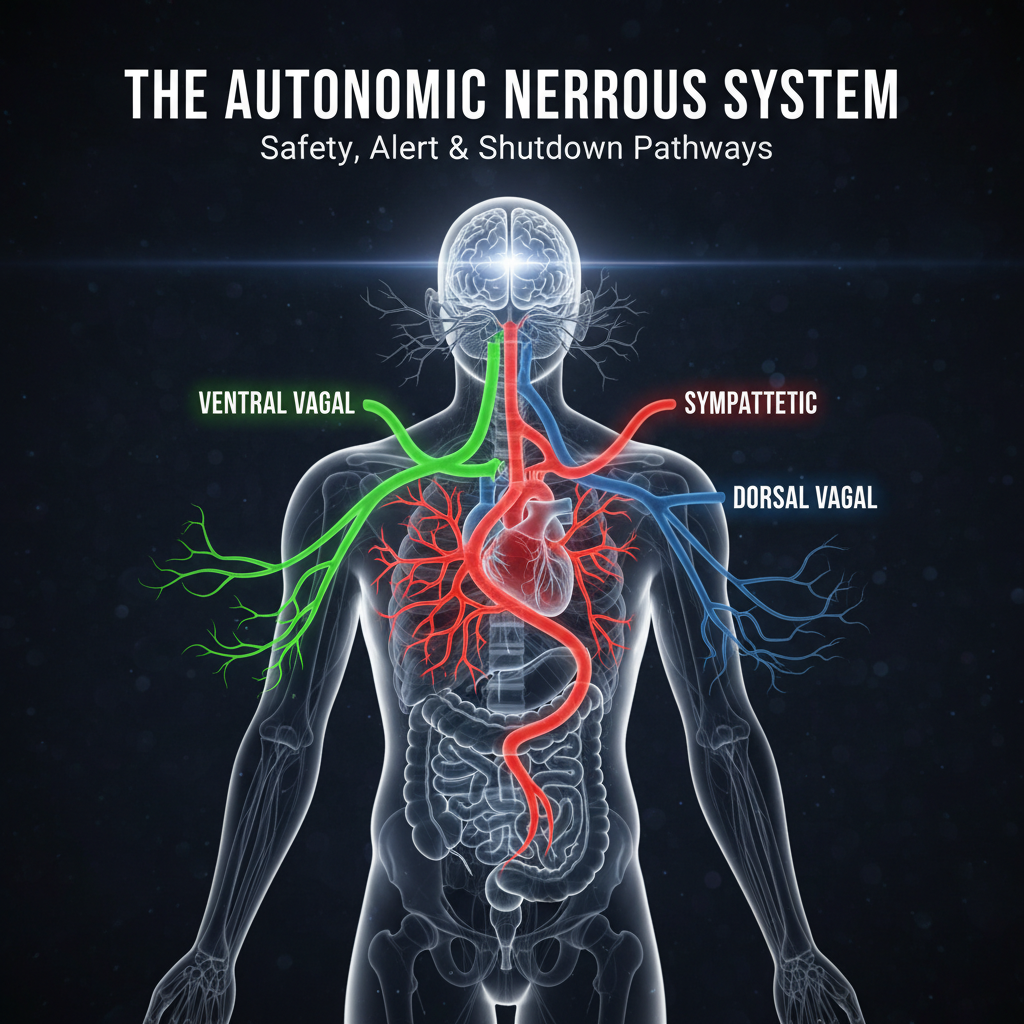
 Stephen Porges' polyvagal theory reveals 3 nervous system states, not 2: Ventral vagal (safety/connection), Sympathetic (fight/flight), Dorsal vagal (shutdown/freeze). Your body decides safety before your conscious mind does—this explains why "calm down" rarely works
Stephen Porges' polyvagal theory reveals 3 nervous system states, not 2: Ventral vagal (safety/connection), Sympathetic (fight/flight), Dorsal vagal (shutdown/freeze). Your body decides safety before your conscious mind does—this explains why "calm down" rarely works
The Old Model vs. Polyvagal Theory
The Traditional View
Before polyvagal theory, we understood the autonomic nervous system as having two branches:
Sympathetic: "Fight or flight" - accelerator Parasympathetic: "Rest and digest" - brake
Simple. Binary. But incomplete.
What Porges Discovered
Porges found that the parasympathetic system has two distinct branches with different functions:
- Ventral vagal (new, "smart" vagus) - social engagement, safety
- Dorsal vagal (old, primitive vagus) - shutdown, immobilization
This means we don't just have an accelerator and a brake—we have three gears.
The Three States
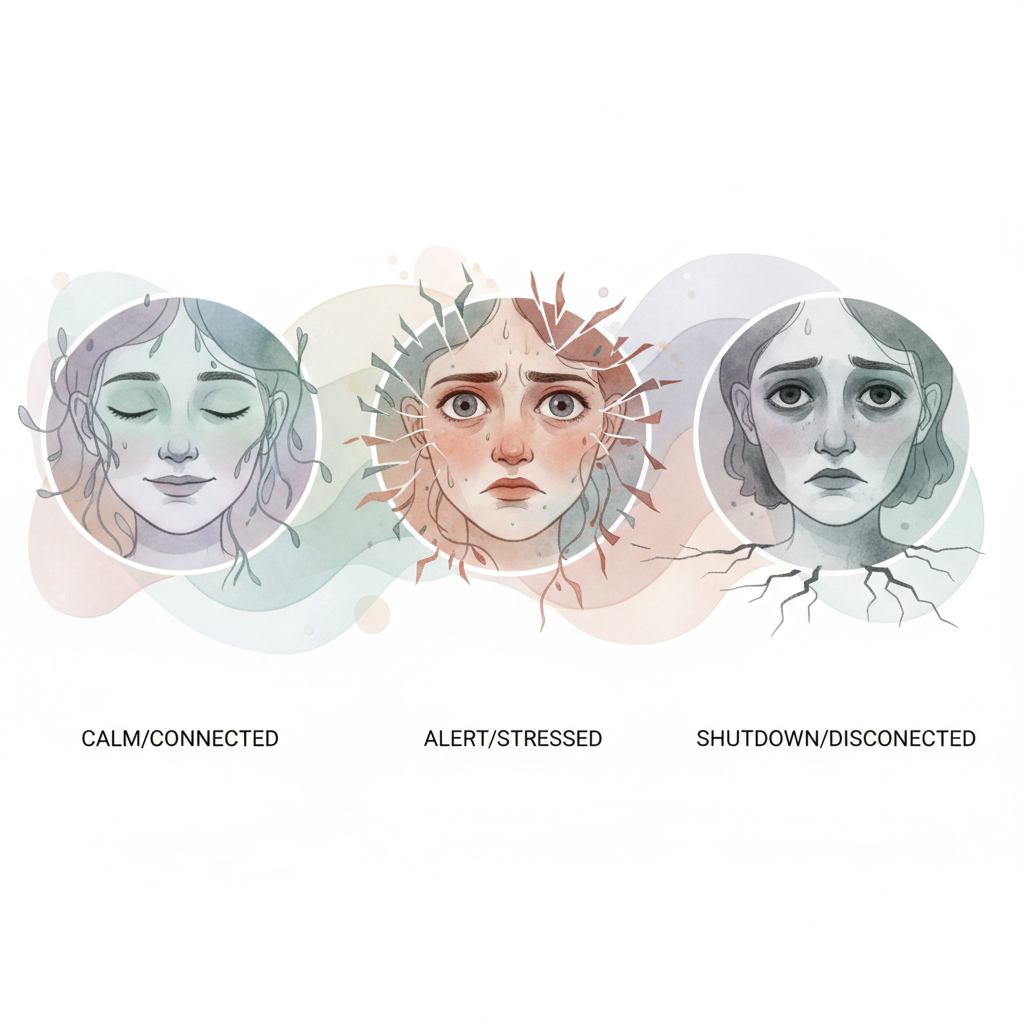 The three states: 1) Ventral vagal (newest, ~200M years)—calm, creative, connected. 2) Sympathetic (~400M years)—alert, mobilized, heart racing. 3) Dorsal vagal (oldest, ~500M years)—shutdown, numb, disconnected. We move up and down this ladder throughout each day
The three states: 1) Ventral vagal (newest, ~200M years)—calm, creative, connected. 2) Sympathetic (~400M years)—alert, mobilized, heart racing. 3) Dorsal vagal (oldest, ~500M years)—shutdown, numb, disconnected. We move up and down this ladder throughout each day
State 1: Ventral Vagal (Safety & Connection)
When you're here:
- Feeling calm and connected
- Open to social interaction
- Creative thinking possible
- Flexible responses
- Recovery happening
Physical signs:
- Relaxed facial muscles
- Soft eye contact
- Regulated breathing
- Stable heart rate
- Digestive function normal
The experience: "I'm safe. I can engage with the world."
State 2: Sympathetic (Fight or Flight)
When you're here:
- Alert to threat
- Mobilized for action
- Heart racing
- Muscles tense
- Focused on survival
Physical signs:
- Rapid heart rate
- Shallow, fast breathing
- Dilated pupils
- Blood flow to muscles
- Digestive shutdown
The experience: "Something's wrong. I need to act."
State 3: Dorsal Vagal (Shutdown)
When you're here:
- Overwhelmed
- Disconnected
- Collapsed energy
- Feeling numb
- Unable to move or think clearly
Physical signs:
- Slowed heart rate
- Flat affect
- Low muscle tone
- Digestive disruption
- Feeling far away
The experience: "I can't handle this. I'm shutting down."
The Hierarchy
These states operate in a hierarchy based on evolutionary development:
Ventral vagal (newest, ~200 million years) - first response when we feel safe
Sympathetic (middle, ~400 million years) - activates when ventral can't handle the threat
Dorsal vagal (oldest, ~500 million years) - last resort when fight/flight won't work
We move up and down this ladder throughout the day, ideally spending most time in ventral vagal.
Neuroception: Your Threat Detector
Here's a crucial concept: neuroception (pronounced "noo-ro-SEP-shun").
Think of it as your body's unconscious threat radar. It constantly scans your environment and internal state for danger signals, all below your conscious awareness—before you even think about a situation.
Your body decides if you're safe before your mind does. This happens in milliseconds, automatically.
This is why:
- You can feel anxious in "safe" situations
- Traumatic stress responses happen automatically
- Telling yourself to "calm down" doesn't work
- Body-based practices (like breathing) can change your state
Neuroception scans:
- Faces and voices (friendly or threatening?)
- Environment (familiar or strange?)
- Internal body state (tense or relaxed?)
Why Breathing Matters in Polyvagal Theory
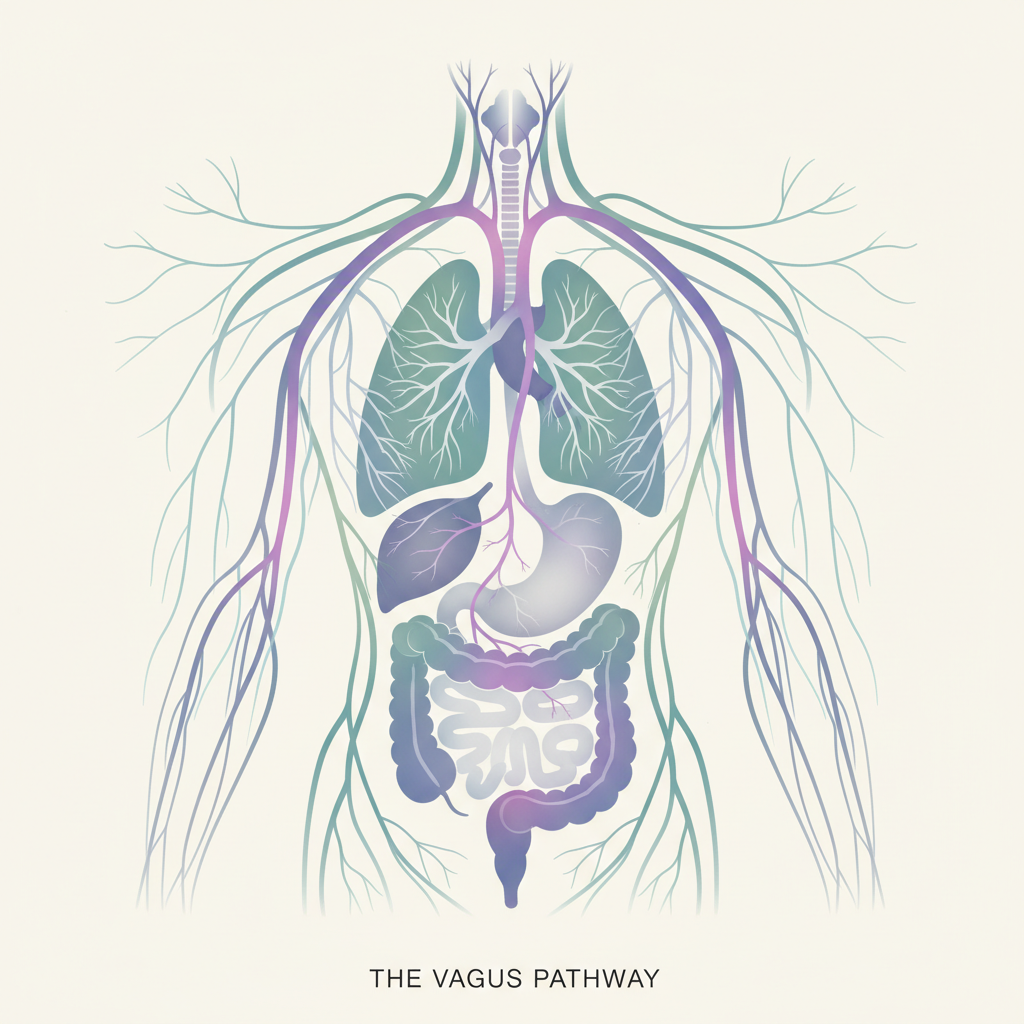
 The vagus nerve connects brainstem to heart, lungs, and gut. Slow exhale = increased vagal tone, lower heart rate, safety signal. Fast inhale/breath hold = sympathetic activation, alertness signal. This is why 4-7-8 breathing (longer exhale) calms while hyperventilation activates
The vagus nerve connects brainstem to heart, lungs, and gut. Slow exhale = increased vagal tone, lower heart rate, safety signal. Fast inhale/breath hold = sympathetic activation, alertness signal. This is why 4-7-8 breathing (longer exhale) calms while hyperventilation activates
The Vagus Nerve Connection
The vagus nerve is the main pathway of the parasympathetic system. It connects your brainstem to your heart, lungs, and gut.
When you exhale slowly:
- Vagal tone increases
- Heart rate decreases
- Blood pressure drops
- You signal safety to your nervous system
When you inhale quickly or hold your breath:
- Sympathetic activation increases
- Heart rate rises
- You signal alertness/threat
Why Exhale Emphasis Works
Breathing techniques that emphasize long exhales work because they directly stimulate the ventral vagal pathway.
This is why:
- 4-7-8 breathing (longer exhale) calms
- Box breathing (equal parts) balances
- Hyperventilation (inhale emphasis) activates
You're not just "relaxing"—you're literally sending a safety signal to your brain through the vagus nerve. Your body understands exhales as "the danger has passed."
Practical Applications
Recognizing Your State
Ask yourself regularly:
- Am I feeling connected or disconnected?
- Is my breath flowing or restricted?
- Can I make eye contact comfortably?
- Do I feel present or far away?
Signs you're leaving ventral vagal:
- Breath becoming shallow
- Jaw or shoulders tensing
- Difficulty focusing
- Urge to flee or freeze
- Losing connection to surroundings
Moving Between States
Sympathetic → Ventral (calming activation):
- Extended exhale breathing (exhale twice as long as inhale)
- Cold water on face (activates diving reflex, vagal)
- Humming or singing (vibrates vagus nerve)
- Safe social connection
- Slow movement
Dorsal → Sympathetic → Ventral (coming out of shutdown):
- Gentle movement first (walking, stretching)
- Orienting to environment (looking around slowly)
- Safe sound and rhythm
- Gradual social engagement
- Avoid forcing rapid change
The Co-Regulation Principle
Here's a key polyvagal insight: we regulate each other.
When a regulated person is present, their nervous system helps calm yours. This is why:
- Babies need caregivers to regulate
- Therapy works partly through the therapist's presence
- Group breathwork can feel more powerful
- Feeling safe with someone helps you relax
This isn't weakness—it's biology.
Polyvagal-Informed Breathwork
 State-based protocols: Sympathetic→Ventral (stressed→calm): 4-8 exhale ratio, cold water on face, humming. Dorsal→Ventral (frozen→engaged): gentle movement first, orient to environment, box breathing 4-4-4-4. Co-regulation is real—other people's nervous systems help regulate yours
State-based protocols: Sympathetic→Ventral (stressed→calm): 4-8 exhale ratio, cold water on face, humming. Dorsal→Ventral (frozen→engaged): gentle movement first, orient to environment, box breathing 4-4-4-4. Co-regulation is real—other people's nervous systems help regulate yours
Protocol for Sympathetic Activation
When you're in fight/flight and need to calm down:
- Acknowledge - Notice the activation without judgment
- Orient - Look around, name what you see
- Breathe - Exhale-focused breathing (4-7-8, or 4-8 ratio)
- Touch - Hand on heart or belly for grounding
- Connect - Soft eyes, relaxed face, think of someone safe
Protocol for Dorsal Shutdown
When you're in freeze/collapse:
- Move gently - Small movements first (wiggle fingers, toes)
- Stand or walk - Very slowly, no force
- Breathe rhythmically - Equal inhale/exhale, box breathing
- Vocalize - Hum, sigh, or speak softly
- Environment - Change location if possible, seek natural light
Daily Ventral Vagal Practice
Maintain your baseline safety state:
-
Morning vagal activation:
- Cold water on face
- Humming while showering
- Extended exhale breathing (5 min)
-
Throughout the day:
- Periodic breath check-ins
- Soft gaze, relaxed jaw
- Movement breaks
-
Before sleep:
- Long exhale breathing
- Gentle stretching
- Safe mental imagery
Criticisms and Limitations
Scientific Debate
Polyvagal theory has critics in the academic community:
Valid critiques:
- Some aspects are oversimplified
- The evolutionary timeline is debated
- "Vagal tone" is more complex than presented
- Not all claims are fully proven
What remains solid:
- The vagus nerve affects heart rate and stress
- Breathing patterns influence autonomic state
- Social connection affects physiology
- Body-based approaches help regulation
Practical Usefulness
Even with scientific debates, polyvagal theory provides:
- A framework for understanding stress responses
- Language for describing nervous system states
- Rationale for why breathwork works
- Guidance for trauma-informed practice
The map isn't perfect, but it's useful.
Key Takeaways
-
Three states, not two: Safety (ventral vagal), activation (sympathetic), shutdown (dorsal vagal)
-
Neuroception happens first: Your body decides safety before your mind analyzes
-
Exhale activates the ventral vagal pathway: This is why slow breathing calms
-
Co-regulation is real: Other people's nervous systems affect yours
-
Movement helps shutdown: You can't think your way out of dorsal, you need to move
-
The goal is flexibility: Being able to move between states appropriately
Understanding your nervous system isn't just intellectual—it's the foundation for all breathwork practice. When you know what state you're in and how to shift it, breathing becomes a precise tool rather than a vague hope.
How to Integrate This Into Your Life
Polyvagal theory sounds great. But how do you actually use it day-to-day?
The 10-Second Check-In
Do this 3 times daily (set an alarm if needed):
- Pause — Stop what you're doing
- Scan — Ask yourself: "What state am I in?"
- Connected, calm, open? → Ventral vagal ✓
- Tense, agitated, racing heart? → Sympathetic
- Empty, disconnected, exhausted? → Dorsal vagal
- Adjust — If needed, use the appropriate technique (see below)
Key check-in moments:
- Upon waking (before checking your phone)
- After lunch
- End of workday
Your State-Based Toolkit
If you're in sympathetic mode (stressed, agitated):
Express technique (2 min):
- Exhale completely
- Inhale 4 seconds through nose
- Exhale 8 seconds through mouth
- Repeat 5-6 times
- Hand on heart, soft eyes
If you're in dorsal mode (frozen, exhausted):
Reactivation technique (5 min):
- Move your fingers, your toes
- Stand up slowly, stretch
- Look around, name 5 objects you see
- Hum or sing something
- Box breathing: 4-4-4-4
Your Daily Vagal Routine
Morning (5 min) — Activate ventral vagal:
- Cold water on face (30 sec)
- Hum in the shower
- 5 minutes of extended exhale breathing
Throughout the day — Maintain the state:
- Regular check-ins
- Relaxed jaw, dropped shoulders
- Movement breaks every hour
Evening (5 min) — Prepare for sleep:
- 4-7-8 breathing (5 cycles)
- Gentle neck and shoulder stretches
- Think of a connection moment from the day
Warning Signs to Recognize
You're leaving ventral vagal when:
- Your breathing becomes shallow
- You clench your jaw without realizing
- You have trouble making eye contact
- You feel a knot in your stomach or throat
- You want to flee a conversation
Immediate action: Long exhale, release your jaw, soften your gaze.
The Power of Co-Regulation
Practice this week:
- Identify 2-3 people who regulate you (you feel calm around them)
- Spend more time with them
- When stressed, call or see one of these people
You can also regulate others:
- Speak more slowly when someone is agitated
- Maintain a soft, open gaze
- Your own regulation is contagious
How to Know You're Progressing
After 2-4 weeks of practice:
- You identify your state more quickly
- You return to calm faster after stress
- You notice warning signs earlier
- Your relationships flow more smoothly
- You sleep better
Ready to track your nervous system state over time? Safe-Flow uses HRV to show you your vagal tone and stress levels, helping you understand how your body responds to breathing practices and daily life—polyvagal theory made measurable.
Join the Beta
Be among the first to experience Safe-Flow. Get early access + exclusive breathing guides.